Antibiotics are medicines that fight bacterial infections in humans and animals. Their mechanism of action is to kill the bacteria or make it difficult for the bacteria to grow and multiply. But they do not work for everything, for example viruses and fungi. Antibiotics can be taken in different ways: orally, topically or intravenously. We should only take antibiotics when required because they can cause side effects and contribute to antibiotic resistance. This happens when the bacteria under goes changes and resists the effects of the antibiotic and thus the bacteria continue to grow.
Discovery of Antibiotics:
Antibiotics have been used to treat infection for several years, although until the last century or so people did not know the infections were caused by bacteria. Various moulds and plant extracts were used by the earliest civilisations to treat infections. Paul Elhrich, a German physician noted that certain chemical dyes coloured some bacterial cells and not others. He concluded that it may be possible to create substances that can kill certain bacteria selectively without harming other cells. In 1909, he discovered that arsphenamine was effective in treating syphilis. This became the first modern antibiotic, although Elhrich referred this treatment as chemotherapy. The word antibiotics was first used 30 years later by Selman Ealksman who in his lifetime discovered more than 20 antibiotics. Alexander Fleming accidentally discovered Penicillin in 1928 when he noticed that the fungus Penicillium notatum had contaminated a culture plate of Staphylococcus bacteria which he had left uncovered. The fungus had created bacteria free zones wherever it grew on plate. Treatment with penicillin was a huge success and thus the US started producing it in mass scale and by the end of World War 2 it was named as the Wonder drug as it saved many lives. Scientists Howard Florey and Ernst Chain shared the 1945 Nobel prize in Medicine with Alexander Fleming for their role in the mass production of Penicillin antibiotic.
Types of antibiotics:
They are broadly classified into 6 groups
- Penicillins: They are used to treat many infections like the skin, urinary tract, chest infections. Eg: Penicillin, amoxicillin, co-amoxiclav, flucloxacillin.
- Cephalosporin: They are used to treat many infections but more effective for serious infections like septicaemia, meningitis. Eg: cephalexin.
- Aminoglycosides: They are used in hospital settings to treat serious illnesses like septicaemia. Eg: gentamycin, Tobramycin.
- Tetracyclines: Used commonly to treat infections of skin like acne and rosacea. Eg: tetracycline, doxycycline, lymecycline.
- Macrolides: It is used to treat lung or chest infections, as an alternative for penicillin allergy or treat penicillin resistant strains of bacteria. Eg: Azithromycin, erythromycin, clarithromycin.
- Fluoroquinolones: It were used to treat wide range of infections like respiratory and urinary tract infections but due to the side effects not commonly used. Eg: ciprofloxacin, levofloxacin.
Other antibiotics are: chloramphenicol for eye and ear infections, fusidic acid for eye and skin infections, nitrofurantoin and trimethoprim for urinary tract infections.
Narrow and Broad Spectrum Antibiotics:
Antibiotics can either have a narrow or broad spectrum of activity. Narrow spectrum antibiotics are more specific and they act only against certain strain and groups of bacteria whereas Broad spectrum antibiotics act upon a wide range of bacteria. Broad spectrum antibiotics are widely used when the knowledge about how to correctly treat an infection is lacking or when the doctors lack time to correctly diagnose the bacteria.
Mode of Actions of Antibiotics:
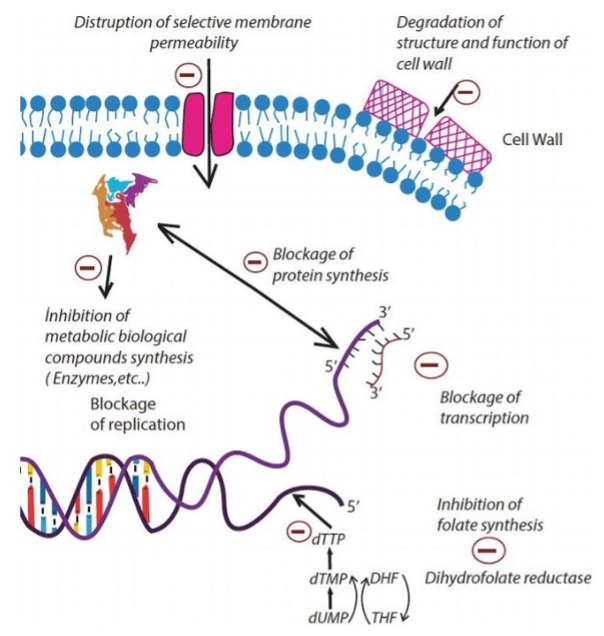
Antibiotic agents used for the treatment of bacterial infections are classified according to their mode of action. There are six major modes of action.
- Interference with cell wall synthesis.
- Inhibition of protein synthesis.
- Interference with nucleic acid synthesis.
- Inhibition of metabolic pathway.
- Inhibition of membrane function.
- Inhibition of ATP synthase.
Thus, according to mechanism of action, the targets of antibacterial drugs include cell membrane, cell wall, protein synthesis, nucleic acid synthesis and biological metabolic compound synthesis. The picture below describes the mode of action of antibiotics.
Side Effects of Antibiotics:
Generally, antibiotics do not cause any side effects if they are used properly. The common side effects are bloating, indigestion, diarrhoea, vomiting, loss of appetite.
Antibiotic Resistance:
Antibiotic resistance happens when bacteria develop the ability to overcome the antibiotic’s ability to kill them and they continue to grow and become resistant to the antibiotics used to treat infections they cause.

Some infections caused by antibiotic resistance bacteria do not respond to any available antibiotics. Antibiotic resistant infections can be severe and potentially life threatening.
Misuse and overuse of antibiotics are the main drivers in promoting growth of drug resistant bacteria.
This is compromising our ability to treat infectious diseases and undermining many advances in medicine.
WHO has declared that antimicrobial resistance is one of the top 10 global public health threats facing the humanity today.It has also changed the slogan of WAAW from Handle Antibiotics with Care to Handle Antimicrobials with Care since 2020 to include broader resistant pathogens to enable the mission to be successful.

The four antibiotic resistant pathogens which are widely reported worldwide are Staphylococcus aureus, Klebsiella Pneumonia, Non- typhoidal Salmonella, and Mycobacterium tuberculosis.
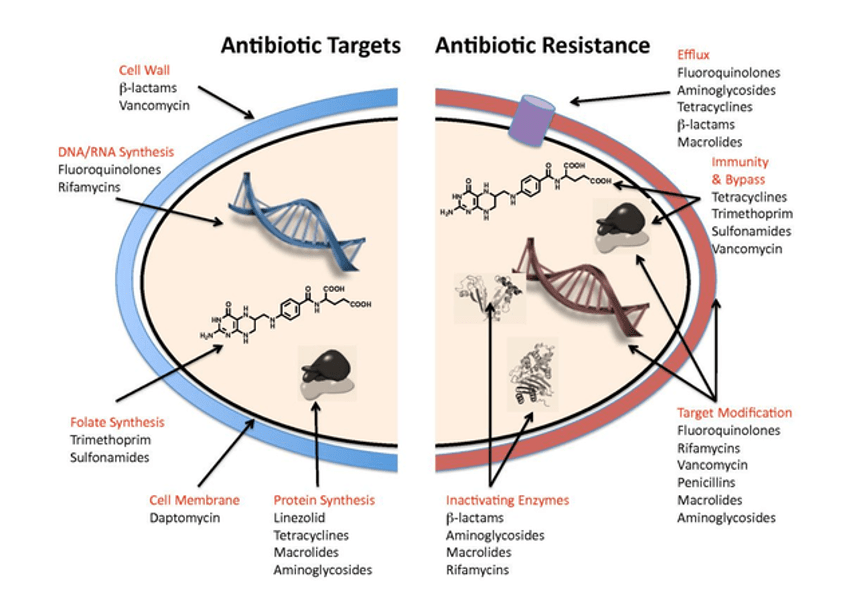
Bacteria develop defence strategies against antibiotics to enhance their survival called as resistance mechanisms.
The different resistance strategies are: restricting the access of the antibiotics by changing entryways, getting rid of the antibiotics using pumps in their cell wall, destroying or changing the antibiotics with enzymes and proteins, bypassing the effects of antibiotics by developing new cell processes, changing the targets for antibiotics.
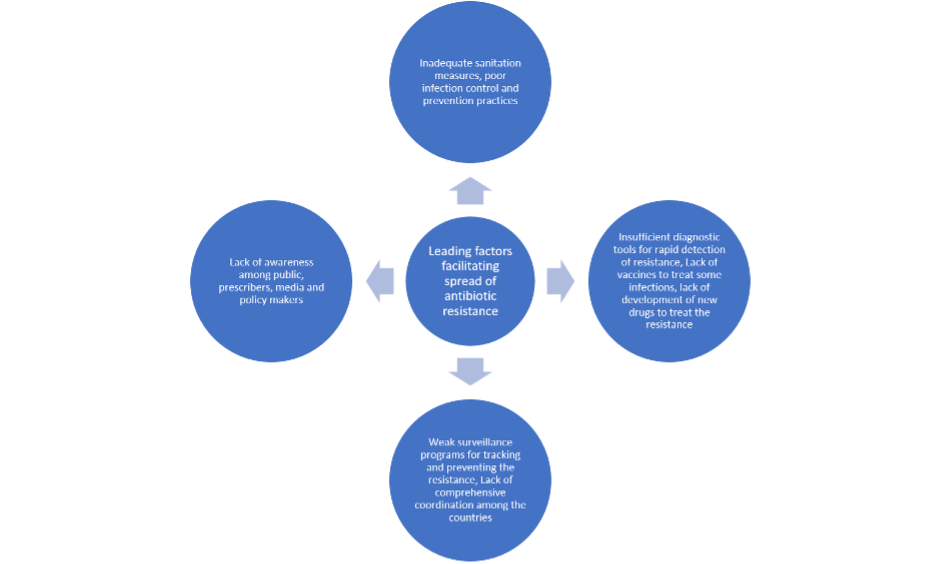
Reasons for Spread of Antibiotic Resistance:
Leading factors facilitating spread of antimicrobial resistance are: lack of awareness about the issue among the public, prescribers, media and policymakers, Inadequate sanitation measures, Poor infection control and prevention practices, Insufficient diagnostic tools for rapid detection of resistance, Lack of vaccines to treat some infections, lack of development of new drugs to treat the resistance, weak surveillance programs for tracking and preventing the resistance, lack of comprehensive coordination among the countries.
Antibiotic resistance contributes to greater morbidity, mortality, disability and economic burdens due to prolonged hospital stays and increased healthcare costs along with decreased societal productivity.

Tackling the antibiotic resistance is of priority and WHO has endorsed the Global Action Plan which focuses to improve the awareness and understanding of antibiotic resistance, to strengthen surveillance and research, to minimise incidence of infection, to optimize the use of antibiotics, to ensure sustainable measures in countering antibiotic resistance.
It has also started the World Antibiotic Awareness week (WAAW), which is held annually every year from 2015 and initiated partnership programs like The Global Antimicrobial Resistance Surveillance system (GLASS), Global Antibiotic Research and Development Partnership (GARDP), Interagency group on antimicrobial Resistance (IACG).

Steps needed to fight Antibiotic Resistance:
We must handle antibiotics with care so they remain effective as long as possible.
Always use antibiotics when prescribed by a certified health professional
Always take the full prescription, even if you feel better.
Never use left- over antibiotics or share them with others.
Health professionals need to ensure that antibiotics are prescribed only when truly needed with right dose and duration.
Policy makers should ensure that surveillance should be improved for antibiotic resistant infections.
Regulate and promote the use of quality medicines
Strengthen policies and implementation of infection prevention and control measures
Research should continue for development of innovative new antibiotics.
Conclusion:
Antibiotic resistance happens when organisms like bacteria develop the ability to defeat the drugs developed to kill them. It has the potential to affect people at any stage of life as well as, healthcare, veterinary and agriculture industries. The growing threat of antibiotic resistance is triggered by biological, behavioural and social factors. Steps need to be taken by the society to reduce the impact and limit the spread of resistance. The world needs to change the way it uses the antibiotics. Even if new antibiotics are developed, without behaviour changes like the vaccination, handwashing, good food hygiene, the antibiotic resistance will remain a major threat to public health. Without urgent steps, we are on the verge of heading into a post antibiotic era, where, minor and common infections can once again kill.
References:
- Frieri M, Kumar K, Boutin A. Antibiotic resistance. Journal of infection and public health. 2017 Jul 1;10(4):369-78.
- MacGowan A, Macnaughton E. Antibiotic resistance. Medicine. 2017 Oct 1;45(10):622-8.
- Levy SB. The challenge of antibiotic resistance. Scientific American. 1998 Mar 1;278(3):46-53.
- Munita JM, Arias CA. Mechanisms of antibiotic resistance. Virulence mechanisms of bacterial pathogens. 2016 Jun 22:481-511.
- Bush K, Courvalin P, Dantas G, Davies J, Eisenstein B, Huovinen P, Jacoby GA, Kishony R, Kreiswirth BN, Kutter E, Lerner SA. Tackling antibiotic resistance. Nature Reviews Microbiology. 2011 Dec;9(12):894-6.


Leave a comment